

17075 Devonshire St., Suite 205 Northridge, CA 91325
Mon - Fri : 9.00 AM - 5.00 PM
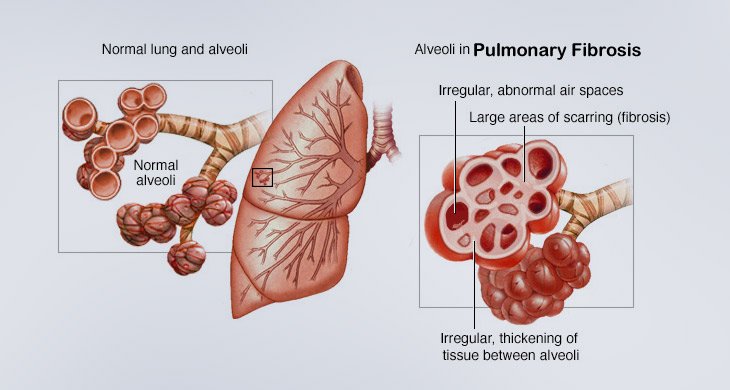
Pulmonary fibrosis literally means scarring of the lungs. The scarring occurs in the interstitium, which is the lung tissue that provides the scaffolding (support structure) for the alveoli (air sacs). Fibrosis thickens the interstitium, making the air sacs stiff so that they are unable to fully expand and hold as much air as they normally should. This thickening also limits passage of oxygen through the wall of the alveoli into the bloodstream. Over time, fibrosis can worsen to the point that patients may need supplemental oxygen to raise low blood oxygen levels, relieve shortness of breath, and improve exercise ability.
Pulmonary fibrosis can happen for many different reasons, including autoimmune disorders, environmental or occupational exposures, as a side effect of certain medications, and a variety of other causes. In many cases, despite extensive evaluation, the cause is unknown; we call such cases idiopathic. It is important that you have a full evaluation by an experienced lung specialist to rule out other causes of pulmonary fibrosis before being diagnosed with idiopathic pulmonary fibrosis (or IPF). While the cause of IPF is unknown, it is a form of pulmonary fibrosis, and specific criteria must be met before the diagnosis of IPF is made.
IPF is usually diagnosed in people between the ages of 50 and 80 years. IPF is very uncommon in people under the age of 50 years. Men are at higher risk than women. A past or current history of smoking cigarettes or working in a dusty environment also increases the risk of developing IPF. IPF sometimes runs in families, and there are several genes associated with its development.
IPF is a rare disease, but it is still common enough that you may know someone with this diagnosis. Overall, about 1 out of every 5,000 people has IPF, which equates to about 50,000-100,000 people in the United States, though data from 2015 shows that as many as 200,000 people may be living with the disease. IPF is much more common in older age groups. In people over 65 years of age, up to 1 out of every 200 people have IPF.
The main symptom of IPF is shortness of breath with activity, which exists in almost everyone as the disease progresses. In fact, in IPF, shortness of breath often limits physical activity. People with IPF may have to slow down, rest and recover throughout an activity or even give up physical activities they once did with ease. Many people with IPF notice they have the most trouble walking quickly, climbing stairs, or going up inclines. About 85% of people with IPF will have a cough. The most frequently occurring symptoms of IPF (shortness of breath, cough and fatigue) are also typical symptoms of other more common diseases; thus, other more common conditions may need to be ruled out before a diagnosis of IPF is made. By definition, IPF affects only the lungs. If a person has joint stiffness or inflammation, rash, or symptoms coming from outside the lungs, then another condition might be present that requires special testing. In the late stages of the disease, IPF can put a strain on the right side of the heart. This is called pulmonary hypertension, which can be associated with swelling in the ankles and worse lung symptoms.
The diagnostic evaluation begins with a thin slice chest CT scan (computerized x-ray imaging). A pulmonologist (lung specialist) with specific expertise in pulmonary fibrosis will review your symptoms, medical history, past medication use, and occupational history. Potential exposures that cause lung scarring in the home or workplace will be discussed. A history of pulmonary fibrosis in other family members is an important clue to the diagnosis. Often your doctor will hear crackles in your lungs when listening with a stethoscope.
Your doctor should also send you for blood tests that can be used to identify blood markers of autoimmune diseases. Currently, there is no single blood test or genetic test to diagnose IPF. Pulmonary function tests (breathing tests) and tests of oxygen levels (e.g., walking tests) are often used to rate the severity of IPF and to look for worsening over time, but these are not helpful in actually diagnosing IPF, as they can be abnormal in other conditions as well. An echocardiogram (ultrasound of the heart) can be used in more advanced IPF to evaluate whether there are any heart complications, such as pulmonary hypertension. Some people will need additional tests to make a diagnosis, including flexible bronchoscopy or a surgical lung biopsy. Bronchoscopy is a procedure in which a thin flexible tube is passed into the lungs through the mouth or nose usually done when a person is sedated (asleep). Samples can be taken through this tube that can be sent for various tests. A surgical lung biopsy is a more invasive procedure in which two or three small incisions are made in the side of the chest under general anesthesia. During this procedure, a surgeon takes two or three samples of lung tissue that can be looked at under a microscope. Making a final diagnosis of IPF typically requires a lung specialist who has experience in evaluating and treating patients with pulmonary fibrosis. Patients are also usually discussed in a multidisciplinary conference, in which various clinical features, imaging findings, and biopsy results are reviewed in a group discussion. This discussion most often includes a pulmonologist, radiologist, and pathologist.
IPF is a serious disease. Most people with IPF will have shortness of breath, exercise limitation, and cough as the disease progresses. Many people will require oxygen at some point in their life. On average, IPF shortens a person’s life. In previous studies, half of people with IPF live less than 3-5 years, and half live longer than 3-5 years. Some people may have lung transplantation for advanced disease. Over the last decade, advances in the management of IPF have improved the outlook for patients. There are FDA medications approved for IPF and many clinical trials attempting to find new therapies.

Bronchoscopy (bron-kos’ko-pi) is a procedure that is done to look at the breathing passages of the lungs (called “airways”).
Learn More
The six-minute-walk test (6MWT) is a common exercise or stress test. This test measures how far you can walk in 6 minutes while reporting how you feel.
Learn More
A pulmonary evaluation is a medical assessment of the respiratory system, specifically the lungs, and airways. This evaluation may be performed...
Learn More